Abstract

Introduction: Recent advances in hematopoietic stem cell transplantation (HSCT) have improved the survival duration in patients who have undergone allogeneic HSCT, and accordingly, late-onset cardiovascular dysfunction is a major problem. Although the ejection fraction (EF) is the most useful parameter of cardiac function, heart failure with preserved EF (HFpEF), the prognosis of which is nearly the same as that of reduced EF, also exists. Recently, global longitudinal strain (GLS), which is more sensitive than the EF in detecting cardiac dysfunction, has been proposed as a new parameter of cardiac function determined using echocardiography. However, validity of GLS in monitoring patients who underwent allogeneic HSCT remains to be evaluated. Therefore, we evaluated long-term cardiac function in patients who had undergone allogeneic HSCT based on GLS and EF using echocardiography.
Patients and Methods: We retrospectively reviewed the medical records of 85 patients (median age, 49 years; range, 17-69 years) with various hematological disorders who underwent allogeneic HSCT between April 2013 and March 2020 at Kobe University Hospital. The diagnoses included acute myeloid leukemia (AML; n = 37), acute lymphoblastic leukemia (n = 13), myelodysplastic syndromes (MDS; n = 5), malignant lymphoma (n = 22), and others (n = 8). Twenty-four patients received a transplant from a related donor (bone marrow, n = 10; peripheral blood, n = 4), while 61 received a transplant from an unrelated donor (bone marrow, n = 25; cord blood, n = 32; peripheral blood, n = 4). Graft-versus-host disease prophylaxis included cyclosporine-based (n = 14) or tacrolimus-based (n = 71). The conditioning regimens were myeloablative (n = 43) or reduced-intensity regimens (n = 42). We assessed the EF, GLS, and cardiac function using echocardiography at baseline (before transplantation) and 1, 3, and 5 year(s) after transplantation. The median cumulative anthracycline dose was 200 mg/m 2 (range; 0-786 mg/m 2). Patients with relapsed or refractory AML received more anthracycline doses, while patients with natural killer/T-cell lymphoma, aplastic anemia, and MDS did not receive anthracycline. We also investigated newly diagnosed cardiovascular events after HSCT. Cardiac events were defined as the development of hypertension, arrhythmia, and heart failure requiring medication or intervention. Further, we analyzed the effect of prescription of cardioprotective agents such as beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers.
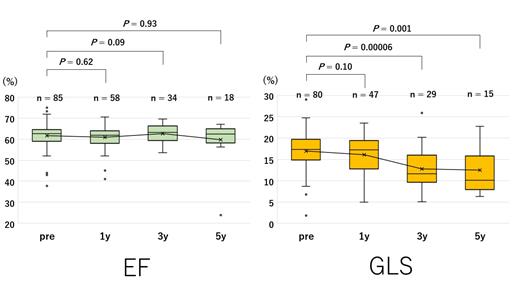
Results: The median follow-up duration in surviving patients was 1647 days (range; 88-2819). The overall survival rate at 5 years was 54.6%, and the causes of death were disease progression (n = 20), sepsis (n = 12), and renal failure (n = 3). None of the patients were hospitalized or died because of cardiac events. EF and GLS 1 year after transplantation were equivalent to those at baseline; however, GLS 3 years after transplantation was significantly decreased compared to that at baseline (P = 0.00006), although the EF did not change (Figure). The median decrease in GLS between baseline and 3 years after transplantation was 4.8% (range; -7.3% to 20.1%). Moreover, patients taking cardioprotective agents (n = 23) had a better GLS at 5 years than that at 3 years; median GLS changed from 10.9% at 3 years to 14.6% at 5 years, while median GLS of the other patients decreased from 11.6% to 8.9%. This suggests that cardioprotective drugs may improve cardiac function. Twenty-four patients (28%) developed newly diagnosed cardiovascular events, which occurred bimodally; 18 patients developed events within 1 year, and the others developed events beyond 4 years. The former tended to have hypertension or arrhythmia, whereas the latter had cardiac dysfunction. Patients who received more than 200 mg/m 2 of anthracycline tended to have slightly more cardiac events than those who received less than 200 mg/m 2 (P = 0.06).
Conclusion: GLS after allogeneic HSCT significantly decreased, although the EF did not change. It is suggested that GLS is a more useful and sensitive parameter than the EF in patients undergoing long-term follow-up after allogeneic HSCT. Additionally, this study indicated that taking cardioprotective drugs may improve cardiac dysfunction after HSCT.
Yakushijin: Nippon Shinyaku: Honoraria; Jazz pharmaceuticals: Research Funding; Chugai pharmaceutical Co. Ltd.: Research Funding. Tanaka: AstraZeneca: Honoraria; Ono pharmaceutical: Honoraria. Matsuoka: Takeda Pharmaceutical Company: Research Funding; Sysmex: Research Funding. Minami: Bayer Yakuhin: Honoraria, Research Funding; Boehringer Ingelheim: Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; Chugai Pharmaceutical: Honoraria, Research Funding; DaiichiSankyo: Honoraria, Research Funding; Eisai: Honoraria, Research Funding; Kyowa-Kirin: Honoraria, Research Funding; Merck Serono: Honoraria, Research Funding; MSD: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Ono Pharmaceutical: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding; Sanofi: Honoraria, Research Funding; Takeda Pharmaceutical: Honoraria, Research Funding; Taiho Pharmaceutical: Honoraria, Research Funding; Eli Lilly: Honoraria, Research Funding; Asahi-Kasei Pharma: Research Funding; Astellas Pharma: Research Funding; Nippon Shinyaku: Research Funding; Yakult Honsha: Research Funding; CSL: Research Funding; Behring: Research Funding; Nippon Kayaku: Research Funding; Celgene: Honoraria; Ohtsuka Pharmaceutical: Honoraria; Shire Japan: Honoraria; Genomic Health: Honoraria; Abbvie: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal